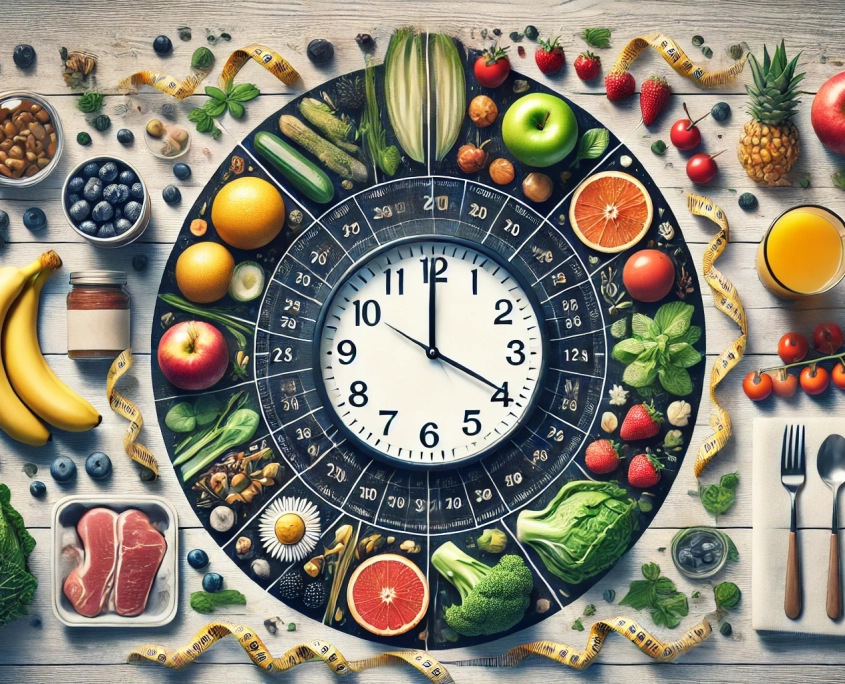
Exploring Various Methods and Their Benefits for Optimal Health
Intermittent fasting (IF) has gained popularity as an effective and sustainable approach to improving health, enhancing metabolic function, and promoting weight loss. This comprehensive guide explores the most popular intermittent fasting methods, providing detailed information to help you choose the best approach for your lifestyle and health goals.
1. The 16/8 Method
Overview:
- The 16/8 method involves fasting for 16 hours and eating all your meals within an 8-hour window each day.
How to Implement:
- Common eating windows are 12 PM to 8 PM or 10 AM to 6 PM.
- During the fasting period, only consume non-caloric beverages like water, herbal tea, or black coffee.
Benefits:
- Simple and easy to integrate into daily life.
- Supports weight loss and improved metabolic health.
- May enhance mental clarity and focus.
2. The 5:2 Method
Overview:
- The 5:2 method involves eating normally for five days of the week and significantly reducing calorie intake on two non-consecutive days.
How to Implement:
- On fasting days, limit caloric intake to 500-600 calories.
- Fasting days should be spaced out (e.g., Monday and Thursday).
Benefits:
- Flexible and less restrictive than daily fasting.
- Promotes weight loss and metabolic improvements.
- Easier to maintain long-term compared to continuous calorie restriction.
3. The Eat-Stop-Eat Method
Overview:
- This method involves fasting for a full 24 hours once or twice a week.
How to Implement:
- Choose one or two non-consecutive days per week to fast completely from dinner to dinner or breakfast to breakfast.
- During the fasting period, only consume non-caloric beverages.
Benefits:
- Encourages significant calorie reduction.
- Can lead to rapid weight loss.
- May improve insulin sensitivity and reduce inflammation.
4. Alternate-Day Fasting
Overview:
- Alternate-day fasting involves alternating between fasting days and regular eating days.
How to Implement:
- On fasting days, either consume no calories or limit intake to about 500 calories.
- Eat normally on the non-fasting days.
Benefits:
- Effective for weight loss and fat loss.
- Can improve various markers of metabolic health.
- Suitable for individuals who can handle more rigorous fasting schedules.
5. The Warrior Diet
Overview:
- The Warrior Diet involves eating small amounts of raw fruits and vegetables during the day and consuming one large meal at night within a 4-hour window.
How to Implement:
- Fast for 20 hours during the day, allowing small snacks of raw fruits and vegetables.
- Eat a large, balanced meal in the evening.
Benefits:
- Aligns with natural human eating patterns.
- Can promote muscle gain and fat loss.
- Encourages consumption of nutrient-dense foods.
6. Spontaneous Meal Skipping
Overview:
- This flexible approach involves skipping meals occasionally when you’re not hungry or too busy to eat.
How to Implement:
- Listen to your body and skip meals when it feels natural.
- Ensure that skipped meals do not lead to overeating later.
Benefits:
- Extremely flexible and easy to follow.
- Reduces overall caloric intake without strict schedules.
- Can improve metabolic flexibility.
Benefits of Intermittent Fasting
-
Weight Loss and Fat Loss:
- Reduces overall calorie intake.
- Increases fat burning and preserves muscle mass.
-
Improved Metabolic Health:
-
- Enhances insulin sensitivity and lowers blood sugar levels.
- Reduces inflammation and oxidative stress.
-
Mental Clarity and Focus:
- Increases levels of brain-derived neurotrophic factor (BDNF).
- May protect against neurodegenerative diseases.
-
Longevity and Cellular Health:
- Promotes autophagy, the body’s process of cleaning out damaged cells.
- May extend lifespan and reduce the risk of chronic diseases.
Considerations for Women
Intermittent fasting can impact women differently due to hormonal fluctuations throughout the menstrual cycle. It is important to tailor fasting practices to suit these physiological differences.
Key Points:
-
Menstrual Cycle Considerations: Women may find it beneficial to avoid prolonged fasting during the luteal phase (post-ovulation to menstruation) when the body requires more nutrients to support hormonal balance.
-
Shorter Fasting Windows: Using shorter fasting periods like the 14/10 method (14 hours fasting, 10 hours eating) can help maintain hormonal balance.
-
Flexibility and Adaptation: Listen to your body and adjust fasting schedules as needed. If you experience adverse effects such as fatigue or hormonal imbalances, consider reducing the fasting duration or frequency.
-
Nutrient-Dense Foods: Focus on consuming nutrient-rich foods during eating windows to support overall health and hormonal balance. Include healthy fats, proteins, and a variety of vegetables.
Expert Insight: Dr. Mindy Pelz, a renowned expert on fasting, emphasizes the importance of aligning fasting practices with women’s hormonal cycles. Her book, “Fast Like a Girl,” provides detailed guidance on how women can safely and effectively incorporate intermittent fasting into their routines.
Choosing the Right Method
Selecting the best intermittent fasting method depends on your lifestyle, health goals, and personal preferences. Here are some factors to consider:
-
Lifestyle Compatibility: Choose a method that fits your daily routine and social commitments.
-
Health Goals: Consider your primary goals, whether they are weight loss, improved metabolic health, or mental clarity.
-
Sustainability: Opt for a method that you can maintain long-term without feeling overly restricted or stressed.
Intermittent fasting offers a variety of methods to improve health, enhance metabolic function, and promote weight loss.
By understanding the different approaches and their benefits, you can choose the method that best aligns with your lifestyle and health goals.
Whether you prefer the structured routine of the 16/8 method or the flexibility of spontaneous meal skipping, intermittent fasting can be a powerful tool for achieving optimal health.




