Nutrient Support for Joint Health: An Academic Review
Joints are critical components of the musculoskeletal system, allowing for movement where two or more bones meet. Maintaining healthy joints is essential for supporting mobility throughout life.
This paper explores the anatomy and function of joints, common joint problems, and the role of various nutrients in supporting joint health and repair.
Anatomy and Function of Joints
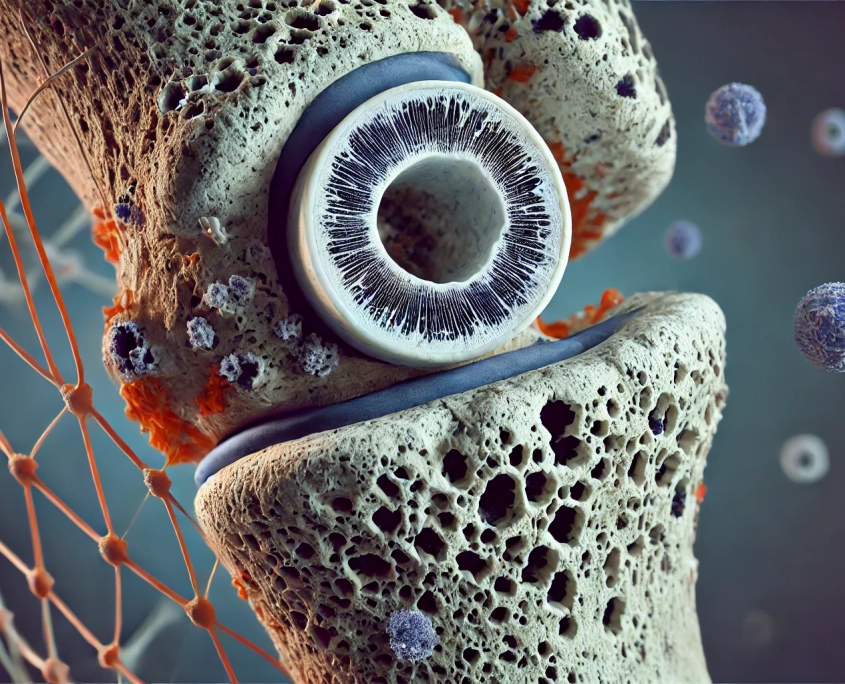
Joint Structure
Joints consist of several components, each contributing to movement and stability:
- Cartilage covers the surface of bones at a joint, reducing friction during movement.
- Chondrocytes produce collagen and the extracellular matrix that support cartilaginous tissues.
- Synovial membrane lines and seals the joint capsule, secreting synovial fluid for lubrication.
- Ligaments are tough connective tissues that connect bones and limit movement.
- Tendons attach muscles to bones, controlling joint movement.
- Bursas are fluid-filled sacs that cushion the friction in a joint.
Types of Joints
Joints vary in their movement capabilities:
- Ball-and-socket joints allow movement in all directions.
- Saddle joints permit back-and-forth and side-to-side movements.
- Hinge joints enable bending and straightening.
- Pivot joints allow limited rotation.
- Planar joints facilitate gliding movements.
- Condyloid joints support various movements except pivotal ones.
How Joints Work
Movable joints are controlled by the contraction and relaxation of muscles attached to bones on either side of the joint. Synovial fluid in the joint cavity helps surfaces glide smoothly and absorbs shock by distributing pressure. Prolonged immobility can cause joint capsules to shrink, reducing mobility.
Common Joint Problems and Their Impact on Quality of Life
Joint problems can arise from acute injuries or chronic conditions. Acute issues, such as dislocations and fractures, typically heal with rest but may have long-term consequences. Chronic conditions, like arthritis, involve inflammation leading to irreversible bone and cartilage damage.
Types of Arthritis
- Osteoarthritis (OA): The most common form, characterized by subchondral bone remodeling, synovial inflammation, and cartilage loss. Inflammatory cytokines stimulate degrading enzymes, causing further damage and pain.
- Rheumatoid arthritis: An autoimmune condition causing joint inflammation and damage.
- Psoriatic arthritis: Associated with psoriasis, leading to joint inflammation and damage.
Oxidative stress can activate cartilage signaling pathways and disrupt chondrocyte homeostasis in OA, resulting in chronic pain, loss of function, and reduced quality of life.
Nutrient Support for Joints
Collagen
Collagen is the primary protein in the extracellular matrix, providing structural support. Several types of collagen exist, each with unique properties. Collagen supplementation can promote connective tissue synthesis, with native type II collagen being particularly effective in OA repair. Clinical studies show that collagen supplementation can relieve pain and improve joint function.
Glucosamine and Chondroitin Sulfate
Glucosamine and chondroitin sulfate are commonly used to manage osteoarthritis due to their roles in cartilage synthesis and maintenance. Meta-analyses indicate glucosamine alleviates joint stiffness, while chondroitin sulfate reduces pain and improves function.
Omega-3 Fatty Acids
Omega-3 fatty acids have strong anti-inflammatory effects, supporting joint health by maintaining a healthy lipid profile in articular cartilage. Clinical studies suggest that omega-3 supplementation can reduce inflammation, relieve pain, and improve joint function.
Vitamin D
Vitamin D regulates bone metabolism and may influence joint health through endocrine and direct effects on inflammation and cytokine synthesis. Low vitamin D status is associated with poor joint health and OA progression. Supplementation can improve muscle strength, reduce pain, and enhance joint function.
Vitamin C
Vitamin C supports immune function, acts as an antioxidant, and is essential for collagen synthesis. It helps maintain oxidative balance in joints and supports the healing of bones, tendons, and ligaments. Long-term supplementation may protect against OA development.
Methylsulfonylmethane (MSM)
MSM is a rich source of sulfur, crucial for cartilage health. It supports joint health by promoting osteoblast differentiation, regulating gene expression, and exhibiting anti-inflammatory and antioxidant effects. Clinical studies show MSM can relieve joint pain and improve joint health.
Emerging Nutrients and Novel Approaches
Hyaluronic Acid
Hyaluronic acid (HA) is found in synovial fluid and connective tissues, providing lubrication and shock absorption. Injectable HA relieves OA pain and may help regenerate cartilage. Supplemental HA also shows promise in improving joint health and reducing pain.
Curcumin
Curcumin, found in turmeric, has strong anti-inflammatory and antioxidant properties. Studies indicate curcumin can improve physical performance and reduce OA symptoms, making it a well-tolerated alternative to NSAIDs.
Boswellia Serrata
Boswellia serrata, or Indian Frankincense, has anti-inflammatory, anti-arthritic, and analgesic properties. Clinical trials demonstrate its effectiveness in reducing inflammation, pain, and improving joint function.
Incorporating Nutrients into Your Diet
A healthy diet, such as the Mediterranean Diet, is rich in nutrients beneficial for joint health. This diet includes seafood (omega-3 fatty acids), fruits, and vegetables (vitamins C and D). Supplementation remains essential for bioactive compounds like MSM, glucosamine, and chondroitin.
Nutrient support plays a crucial role in maintaining joint health and managing joint problems. Collagen, glucosamine, chondroitin sulfate, omega-3 fatty acids, vitamins D and C, MSM, hyaluronic acid, curcumin, and Boswellia serrata have all shown promise in supporting joint health and alleviating symptoms of joint conditions. A combination of a nutrient-rich diet and appropriate supplementation can enhance joint function, reduce pain, and improve quality of life for individuals with joint issues.
References
- Barron, K. (2024). A Clinical Exploration of Nutrient Support for Joints. Wholistic Matters.
- Arthritis Foundation. (2024). arthritis.org.
- National Institute of Arthritis and Musculoskeletal and Skin Diseases. (2024). niams.nih.gov.
- Felson, D. T., et al. (2000). Osteoarthritis: New Insights. Part 1: The Disease and Its Risk Factors. Annals of Internal Medicine, 133(8), 635-646.
- Abramson, S. B. (2008). Osteoarthritis and Nitric Oxide. Osteoarthritis and Cartilage, 16, S15-S20.
- Berenbaum, F. (2013). Osteoarthritis as an Inflammatory Disease (OSTEOARTHRITIS IS NOT OSTEOARTHROSIS!). Osteoarthritis and Cartilage, 21(1), 16-21.
- Bello, A. E., & Oesser, S. (2006). Collagen Hydrolysate for the Treatment of Osteoarthritis and Other Joint Disorders: A Review of the Literature. Current Medical Research and Opinion, 22(11), 2221-2232.
- Vlad, S. C., et al. (2007). Glucosamine for Pain in Osteoarthritis: Why Do Trial Results Differ? Arthritis & Rheumatology, 56(7), 2267-2277.
- Sengupta, K., et al. (2010). A Double Blind, Randomized, Placebo Controlled Study of the Efficacy of an Extract of Boswellia serrata in the Management of Osteoarthritis of the Knee. International Journal of Medical Sciences, 7(6), 366-377.
- Henrotin, Y., et al. (2009). Biological Actions of Curcumin on Articular Chondrocytes. Osteoarthritis and Cartilage, 17(2), 274-283.
- Messier, S. P., et al. (2009). Effects of Intensive Diet and Exercise on Knee Joint Loads, Inflammation, and Clinical Outcomes Among Overweight and Obese Adults with Knee Osteoarthritis: The IDEA Randomized Clinical Trial. JAMA, 310(12), 1263-1273.
- Hunter, D. J., & Bierma-Zeinstra, S. (2019). Osteoarthritis. The Lancet, 393(10182), 1745-1759.
- Dawson, J. K., et al. (2002). Epidemiology of Chronic Inflammatory Joint Disease. Best Practice & Research Clinical Rheumatology, 16(5), 685-704.
- Haq, I., et al. (2003). Vitamin D and Its Role in Osteoarthritis. Journal of Clinical Rheumatology, 9(5), 232-238.
- McAlindon, T. E., et al. (2013). Effect of Vitamin D Supplementation on Progression of Knee Pain and Cartilage Volume Loss in Patients with Symptomatic Osteoarthritis: A Randomized Controlled Trial. JAMA, 309(2), 155-162.
- Vimaleswaran, K. S., et al. (2013). Association of Vitamin D Status with Arterial Blood Pressure and Hypertension Risk: A Mendelian Randomisation Study. The Lancet Diabetes & Endocrinology, 2(9), 719-729.
- Clegg, D. O., et al. (2006). Glucosamine, Chondroitin Sulfate, and the Two in Combination for Painful Knee Osteoarthritis. New England Journal of Medicine, 354(8), 795-808.
- Hochberg, M. C., et al. (2011). American College of Rheumatology 2012 Recommendations for the Use of Nonpharmacologic and Pharmacologic Therapies in Osteoarthritis of the Hand, Hip, and Knee. Arthritis Care & Research, 64(4), 465-474.
- Wandel, S., et al. (2010). Effects of Glucosamine, Chondroitin, or Placebo in Patients with Osteoarthritis of Hip or Knee: Network Meta-Analysis. BMJ, 341, c4675.
- Van Spil, W. E., et al. (2013). Osteoarthritis Phenotypes and Their Implications for Pathophysiology and Treatment. Current Opinion in Rheumatology, 25(5), 562-568.
- Chua, C. C., et al. (2008). Effects of Vitamin C on Extensor Tendon Healing in a Chicken Model. American Journal of Sports Medicine, 36(5), 967-973.
- Hemilä, H. (1997). Vitamin C and the Common Cold. British Journal of Nutrition, 77(1), 59-72.
- Nimni, M. E. (1983). Collagen: Structure, Function, and Metabolism in Normal and Fibrotic Tissues. Seminars in Arthritis and Rheumatism, 13(1), 1-86.
- McAlindon, T. E., et al. (2000). The Vitamin C Intake and the Risk of Developing Knee Osteoarthritis: Data from the First National Health and Nutrition Examination Survey (NHANES I). Annals of the Rheumatic Diseases, 59(11), 808-813.
- Wang, Y., et al. (2014). Association Between Dietary Intake of Antioxidants and Prevalence of Knee Osteoarthritis: Data from the Osteoarthritis Initiative. Annals of the Rheumatic Diseases, 73(9), 1673-1679.
- Hunter, D. J., et al. (2015). Longitudinal Analysis of Vitamin D Levels and Joint Pain in Older Adults. Journal of Clinical Endocrinology & Metabolism, 100(5), 1969-1977.
- Ameye, L. G., & Chee, W. S. S. (2006). Osteoarthritis and Nutrition. From Nutraceuticals to Functional Foods: A Systematic Review of the Scientific Evidence. Arthritis Research & Therapy, 8(4), R127.
- Kim, L. S., et al. (2006). Efficacy of Methylsulfonylmethane (MSM) in Osteoarthritis Pain of the Knee: A Pilot Clinical Trial. Osteoarthritis and Cartilage, 14(3), 286-294.
- Debbi, E. M., et al. (2011). Efficacy of Methylsulfonylmethane Supplementation on Osteoarthritis of the Knee: A Randomized Controlled Study. BMC Complementary and Alternative Medicine, 11(1), 50.
- O’Connell, T. M. (2006). Methylsulfonylmethane (MSM) Supplementation in the Treatment of Osteoarthritis. Journal of Nutritional Biochemistry, 17(8), 507-510.
- Pagonis, T. A., et al. (2004). The Effect of Methylsulfonylmethane on the Osteoarthritis of the Knee. Clinical Drug Investigation, 24(5), 329-335.
- Fox, B. A., et al. (2009). Viscoelastic Properties of Hyaluronan-Polyethylene Glycol Hydrogels Designed for Articular Cartilage Repair. Biomacromolecules, 10(4), 919-926.
- Reichenbach, S., et al. (2010). Intra-Articular Injections of Hyaluronic Acid for Osteoarthritis of the Knee: A Systematic Review and Meta-Analysis. JAMA, 283(11), 1304-1311.
- Bannuru, R. R., et al. (2009). Efficacy and Safety of Intra-Articular Hyaluronic Acid in the Treatment of Osteoarthritis: A Meta-Analysis. Journal of Bone and Joint Surgery, 91(3), 253-262.
- Henrotin, Y., et al. (2013). Efficacy and Safety of a Curcuma Extract in the Treatment of Patients with Knee Osteoarthritis: A Randomized, Double-Blind, Placebo-Controlled Study. Arthritis Research & Therapy, 15(5), R224.
- Chandran, B., & Goel, A. (2012). A Randomized, Pilot Study to Assess the Efficacy and Safety of Curcumin in Patients with Active Rheumatoid Arthritis. Phytotherapy Research, 26(11), 1719-1725.
- Belcaro, G., et al. (2010). Efficacy and Safety of Meriva, a Curcumin-Phosphatidylcholine Complex, during Extended Administration in Osteoarthritis Patients. Alternative Medicine Review, 15(4), 337-344.
- Panahi, Y., et al. (2014). Effect of Curcuminoids on Inflammatory Markers in Patients with Chronic Kidney Disease: A Randomized Controlled Trial. Journal of Endocrinological Investigation, 37(11), 1157-1163.
- Di Pierro, F., et al. (2013). Clinical Efficacy and Safety of a Fixed Combination of Boswellia serrata Extract and Curcumin Phytosome in Osteoarthritis: A Randomized, Double-Blind, Placebo-Controlled Study. Journal of Nutritional Biochemistry, 24(10), 1653-1659.
- Siddiqui, M. Z. (2011). Boswellia Serrata, a Potential Antiinflammatory Agent: An Overview. Indian Journal of Pharmaceutical Sciences, 73(3), 255-261.
